With so many different theories and models on chronic pain, it can be confusing to fully understand how it works – especially for those who suffer from it. But one such model, known as ‘the pain triangle’, is a simplistic way to view chronic pain, providing patients with a lot of knowledge and potential recovery options.
Understanding pain is an essential aspect of overcoming it. When you know exactly what you’re dealing with, and all the inner workings of it, you have a much more informed way of dealing with it accordingly. Knowledge allows you to make the right decisions for yourself and your individual circumstances and can be highly useful in managing chronic pain. But with so much knowledge and theory on pain out there, how do you wade through it all?
This article will aim to explain the concept of one such theory, known as the pain triangle. When applied to chronic pain, this theory can provide more effective methods of coping, and a better level of understanding.
The term ‘chronic pain’ applies to that which is ongoing and experienced for longer than 3 months. It can be harrowing for those who suffer from it, causing confusion and loneliness. The pain triangle focuses on the connected aspects of this pain and can be an effective way to demonstrate how pain interacts with other parts of ourselves.
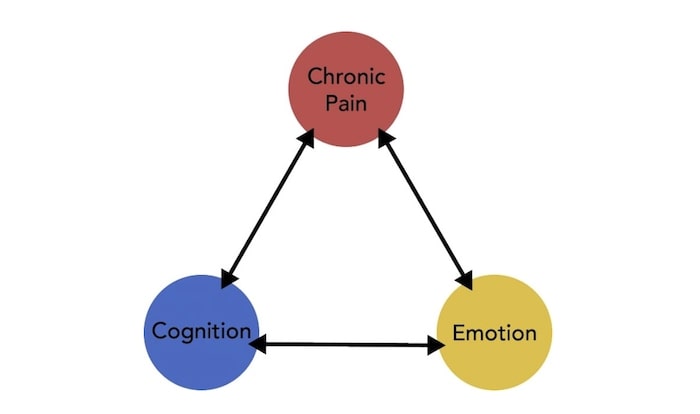
The pain triangle consists of three aspects: pain, cognition, and emotion. To properly understand it, it can be pictured as three points of a triangle, with chronic pain itself sitting at the top, cognition (thoughts and beliefs about the pain), and emotion (feelings about the pain) on either of the bases points. All these points are connected to form the triangle, with chronic pain affecting and causing issues both cognitively and emotionally.
When experiencing chronic pain, can affect cognitive functioning in various ways, manifesting in symptoms such as impaired focus, memory issues, attention problems, and poor executive functioning. Affected cognition can also exacerbate feelings of pain and cause a much more intense sensation. While it’s not yet known whether cognitive issues will show up immediately or much later on in chronic pain sufferers, studies published in the Journal of Pain and Symptom Management found that “42% of patients seeking treatment for chronic pain who had no history of head injury reported at least one cognitive complaint (forgetfulness, difficulty maintaining attention, or difficulty with attention and thinking)”.
The study then goes on to discuss the things that could actually be the cause of these cognitive complaints, such as “neurological disorders, medication is taken to treat the pain, the feeling of pain itself, preoccupation with injuries or ill health, sleep deprivation stressful circumstances and/or other emotional factors, or even a combination of all”. With so many potential causes for cognitive decline, it’s important to be in close contact with your doctor or medical professional during treatment. This way, you can ensure any issues that do come up are noticed and treated quickly.
Emotional aspects of chronic pain include things like feelings of depression, anxiety, anger, frustration, and helplessness. All these negative feelings can serve to heighten the perception of pain even further, while conversely, positive feelings and mindsets have been shown to reduce feelings of pain. Psychological welfare is a serious issue for patients dealing with chronic pain, and it exists on a spectrum that ranges from mild feelings of self-esteem issues and insecurity to much more serious problems such as self-harm and even suicide. When you’re dealing with continuous pain, whether it’s mild or severe, you can experience a whole host of different emotions about it; from anxiety about oncoming, flare-ups to fear of the pain getting worse. Negative self-talk such as “Why is this happening to me?” and” How can I ever cope with this?” are common, and when this sort of negative narrative continues it can be extremely detrimental to someone’s emotional and mental wellbeing.
Both cognitive and emotional issues can impact other areas of a patient’s life as well. When struggling cognitively, one might begin to become forgetful at work, unable to perform to the best of their abilities. And when struggling emotionally, one might begin to inadvertently create issues in their interpersonal relationships, which – if not dealt with – can cause them to become secluded, lonely, and isolated.
When someone is experiencing chronic pain, they’re likely to notice that cognitive/emotional problems exist in a cycle. If the pain flares up, these cognitive/emotional issues get worse. If the pain settles, so do these additional issues. For those who believe they’re in such a cycle, it’s important to understand how to break that cycle. This can be done through various activities such as spending time around loved ones, focusing on religion and/or spirituality, meditating, joining a chronic pain support group, finding distraction through a new hobby, journaling, and positive thinking.
Though the pain triangle might seem like a simple way to view chronic pain, it’s always important to speak with your doctor or medical professional to ensure you’re full of the cause of your chronic pain, as well as how it has the potential to affect your cognitive and emotional functioning. Given that it can often cause mood disorders such as anxiety and depression, it’s essential to discuss not only your pain but any onset of psychological or cognitive issues you may be experiencing. That way, you’ll know whether there are more points of the triangle that needs to be dealt with, other than purely the pain aspect.
Taking the pain triangle into account is a great way to ensure you’ve got a simple yet holistic view of your chronic pain issues, rather than just a spotlight on one particular area – the pain itself. This way, you can ensure you’re covering all your bases and are giving yourself the best chance at rehabilitation.
Precision Pain Care and Rehabilitation has four convenient locations in Richmond Hill – Queens and New Hyde Park, Lindenhurst, and Valley Stream – Long Island. Call the Queens office at (718) 215-1888, or (516) 419-4480 for the Long Island offices, to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.













