What Is The Anterior Cruciate Ligament (ACL)?
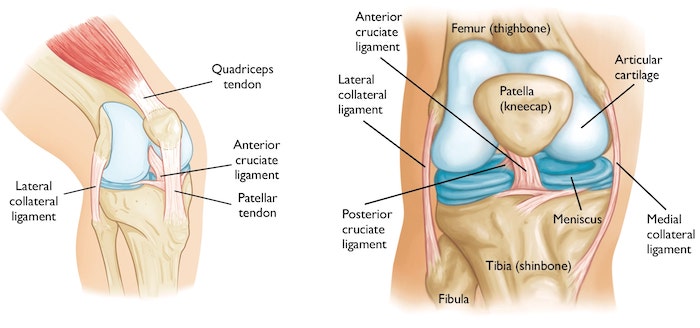
The ACL crosses the posterior cruciate ligament in the center of the knee joint and is part of a group of ligaments that connect the thigh bone (femur) to the lower leg (tibia). These ligaments stabilize and support the knee joint. The ACL prevents the tibia from moving too far forward on the femur. It also keeps the knee from twisting inward excessively.
“Tens of thousands of people tear their ACL and approximately 200,000 operations are performed every year in the US,” says Scott A. Rodeo, MD, team physician for the New York Giants and co-chief emeritus of the Sports Medicine Institute.
“HSS physicians and researchers are working to identify the most effective current treatments in order to develop new therapies that may be even more successful in helping people return to their active lifestyles after ACL injuries.”
What Are The Symptoms And Causes Of A Torn ACL?
A person may hear a popping noise at the time of injury. More commonly, though, the injured athlete notices immediate pain and swelling. The knee may also shift or buckle due to instability, and jumping, landing, and pivoting can cause severe pain.
“ACL injuries are fairly common in the NFL with about two occurring each year in every team,” says Russell F. Warren, MD, New York Giants team physician and attending orthopedic surgeon at HSS. “Partial or complete ACL tears are typically non-contact injuries that occur when a person does a sharp twist-pivot with the foot planted, such as when avoiding a tackle during football or changing direction when landing after a jump in basketball,” Dr. Warren explains.
But it’s not only football players who tear this ligament that is crucial for stabilizing and supporting the knee joint. Athletic individuals of any age - particularly those who play sports requiring a pivoting motion such as soccer, lacrosse, basketball, field hockey, golf, and skiing - are at risk.
“Sports medicine physicians can usually diagnose an ACL injury during the physical exam,” Dr. Rodeo says. “A magnetic resonance imaging (MRI) scan also gives the most accurate anatomic information about the injury, and can reveal whether or not the meniscus and other structures in the knee are still intact.”
Dr. Rodeo explains that women experience ACL injuries more often than men, perhaps owing to a variety of factors including differences in neuromuscular function and anatomical differences. Female basketball players, for example, tend to jump and land with their knees straight and in a knock-kneed position, which could lead to injury.
How Do You Treat ACL Injuries?
The first line of treatment for ACL injury involves resting, icing, and elevating the leg. An anti-inflammatory medication can also decrease pain and swelling, Dr. Rodeo says.
In some cases when people do not require a return to pivoting sports, physical therapy can strengthen the joint without surgery, he explains. With physical therapy, many people can continue to be active at the gym and at intermediate levels of jogging, running, and skiing.
In athletes who play sports that demand constant pivoting, ACL reconstruction surgery may be the best option, Dr. Warren says. Fixing the ACL will prevent abnormal movement of the knee that could cause additional knee damage to the menisci and cartilage. When the ACL is injured, the meniscus cartilage between the femur and tibia absorbs a greater impact and can tear, leading to a greater risk of osteoarthritis development, he explains.
“The key element is the time from injury to surgery,” Dr. Warren says. “The longer the time frame, the more injury is possible to the joint. We prefer to do the surgery earlier rather than later.”
Orthopedic surgeons at HSS perform over 1,200 ACL reconstruction procedures on damaged ligaments each year and have significant experience repairing this injury in young patients. In the past, surgery involved repairing the ligament or using a synthetic material to replace the ligament, but the failure rate was too high, Dr. Warren says.
Though the ligament could heal when the leg was put in a cast for six weeks, the ligament often remained loose and did not stabilize the knee. In addition, when the cast was removed, the knee joint was very weak and stiff. More recently, there has been some renewed interest in repair if the ACL injury occurs directly at the bone attachment rather than in the mid-substance ligament. With improved arthroscopic techniques this may prove to be a viable option.
Today, reconstruction involves replacing the entire ligament with a tendon graft, Dr. Warren says. The graft could come from the injured person’s hamstring tendon, quadriceps tendon, or patellar tendon, which stabilizes the kneecap and has bone on each end. Surgeons can also use an allograft, which is human donor tissue.
The source of the tendon graft depends on the situation. “In older patients, we can use an allograft, but the failure rate is higher with an allograft in younger, more active patients,” Dr. Rodeo explains. “For example, recreational skiers in their 40s and 50s seem to heal well when we use an allograft, but in 20-year-old basketball players, an allograft has up to a 25 percent failure rate.”
At HSS, the surgery is commonly performed using regional epidural anesthesia with light sedation. The procedure is done arthroscopically, through small incisions in the knee, with a combination of fiber optics and small instruments.
People who undergo this procedure can move their knee immediately after surgery and return home the same day. Two days later, physical therapy begins.
“In about four months, people are running,” Dr. Warren says. “In about six to eight months, people who have had ACL reconstruction can actively participate in sports.”
What Research Is Conducted On ACL Injuries And Treatments?
Scientists at HSS have spent decades investigating the function of the ACL and the best methods for repairing injury. Recent efforts have involved understanding ACL injuries and patient experiences through prospective clinical research registries.
“Research registries are a significant area of interest at HSS,” Dr. Rodeo says. “Registries have been and will continue to be a great help for us to learn about what types of ACL procedures perform the best in certain situations—depending on the type of graft, the patient’s age, and the patient’s activity level, among other factors.”
The ACL registry at Special Surgery started in 2008. It currently includes data from over 2,700 patients, including samples of synovial fluid within the knee joint that is being used to examine genes, proteins, and inflammatory cells that could be linked to the development of arthritis. The information in the registry allows researchers to prospectively track clinical data and identify successful methods for treating and preventing injury.
Experts are also working in the laboratory to identify advances in ACL repair. “Hospital for Special Surgery uses a team approach to research, with clinicians, surgeons, basic researchers, physical therapists, and others all working together,” Dr. Warren says.
A challenge of developing new materials for ACL repair involves the fact that the tissue must be able to handle weight-bearing immediately, Dr. Rodeo explains. One area of investigation involves cell-based approaches for generating and healing the tissue, such as with stem cells. In another strategy, artificial ligaments could be made through tissue engineering, as living cells begin to grow on a scaffold.
HSS researchers are also going back to basics. Biomechanics experts are investigating the role of ligaments in stabilizing the knee, and biologists are studying how ligament cells respond to mechanical loads and how they heal after damage.
“We as orthopedic researchers are looking forward to advances in other fields, including materials science and molecular biology, which could lead to clinical applications for treating ACL injuries even more effectively in the future,” Dr. Rodeo says.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens, and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888 or (516) 419-4480 for the Long Island office to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.